Addiction: The Loop Between Pain and Relief
Understanding the Science of Addiction, and How to Unlearn It
Imagine you touch a hot stove. You only need that lesson once. Your brain says, avoid that.
But when you take a drink after a stressful day, or a puff when you’re restless, the brain says, remember that. That’s addiction’s cruel inversion of learning. It’s not a lack of discipline. It’s the brain doing what it evolved to do: repeat what feels rewarding.
The Brain’s Survival Code…Hijacked
Dopamine isn’t a pleasure chemical…it’s a teacher. It stamps experience with a note that says, remember this; it keeps you alive. When something feels good (food, laughter, connection) dopamine marks the moment as important: do this again.
That system once worked beautifully. Find berries → eat → survive.
But the modern world overwhelms that same circuitry. Nicotine, alcohol, and ultra-processed foods trigger dopamine far more powerfully than anything nature designed us to enjoy. The brain can’t tell the difference between what’s necessary and what’s novel, it just learns faster than it can unlearn.
Soon, the brain builds a narrow path: trigger → behavior → relief.
Anxiety → smoke.
Boredom → drink.
Each repetition deepens the groove until it feels automatic, comfort mistaken for safety.
Addiction is learning gone too far. Every use reinforces the message this fixes me, until craving itself becomes the reward. Neuroscientists call this incentive sensitization: the “wanting” system grows louder even as the “liking” fades.
Over time, brain imaging shows the amygdala (our internal alarm)nand the insula (the body’s feeling center) firing as if survival depends on the next drink or drag. Meanwhile, the prefrontal cortex, the part that reasons and resists, goes quiet.
The brain stops asking, Do I like this? and starts insisting, I need this to stay alive.
That’s addiction: a brilliant learning system turned against itself.
Why Quitting Feels Impossible (And Why It Isn’t)
When you try to stop, the loop doesn’t vanish…it fires alarms. Cravings feel like survival threats, not thoughts. That’s why willpower alone feels hopeless; you’re not fighting logic, you’re calming a nervous system that thinks it’s starving.
This is where modern medicine has changed the odds. Medications like naltrexone for alcohol or varenicline for nicotine quiet the brain’s false hunger. They turn down the “reward prediction error”—that dopamine spike of I need it. They don’t erase desire, but they shrink it to a size you can reason with.
That’s why working with your doctor matters. For alcohol, quitting suddenly without medical guidance can trigger dangerous withdrawal: seizures, heart strain, even death. A physician can help you taper safely, prescribe medication, and track labs as your brain recalibrates. Recovery is a biological process before it’s a psychological one.
The Lure Beneath the Craving
Dr. Jud Brewer’s research adds another layer. His brain-imaging studies show that craving isn’t about the substance, it’s about wanting relief. The more we fight an urge, the more we feed it. Resistance keeps the loop alive.
His approach is radical in its simplicity: get curious instead of reactive.
When a craving arises, he teaches patients to pause and notice: What does this feel like in the body? Is it heat, tightness, restlessness? How long does it last?
By turning curiosity toward the craving, you move out of the survival brain (the amygdala) and into the observer brain (the prefrontal cortex). The more you notice, the less urgent it feels. Over time, that awareness becomes the new reward.
Think of it as changing your relationship to the craving instead of fighting it.
You stop being the person drowning in the urge and start being the one noticing the wave.
Why Mindfulness and Medication Work Better Together
Medication turns down the volume. Mindfulness changes the station. Behavioral tools like cognitive-behavioral therapy or digital coaching add rhythm and accountability. Each one targets a different part of the loop:
Medication weakens the chemical reward.
Mindfulness teaches the brain not to chase the relief.
Coaching or CBT rewires daily cues—new coffee mug, new route home, new bedtime ritual.
Layer them, and recovery stops being a fight; it becomes retraining.
Healing is a Skill, Not a Miracle
The brain that learned addiction can unlearn it through repetition, not punishment. Every craving that passes without action is a new data point.
You don’t have to win once; you practice rewiring until the habit loop fades into disuse. That’s neuroplasticity, the brain’s quiet mercy.
But this isn’t a do-it-yourself project. Especially with alcohol or polysubstance use, your physician is part of the team. They can monitor your health, protect you from unsafe withdrawal, and use medications strategically while you practice new skills.
The Takeaway
Addiction isn’t a character flaw. It’s a memory that’s learned too well.
Recovery isn’t about erasing that memory, it’s about teaching the brain a better one: that calm, clarity, and connection are safer rewards than relief.
So if you find yourself reaching again, pause.
Ask what your brain is asking for beneath the craving: rest, connection, safety, or belonging.
Then reach for the thing that actually meets that need.
That’s how the loop unravels. That’s how healing becomes a habit.
*Below you will find Unlearning the Loop: A Guided Practice for Understanding and Rewiring Addiction, a worksheet helps you understand why cravings feel powerful and how to interrupt them safely.
Need Help Now? Here’s Who to Call
(All are free, confidential, and available 24/7 in the U.S.)
For quitting smoking or vaping
1-800-QUIT-NOW (1-800-784-8669)
Connects you to your state’s quitline for free coaching, text support, and nicotine-replacement guidance.
For alcohol or drug use help
SAMHSA National Helpline – 1-800-662-HELP (4357)
A 24-hour line that offers information, emotional support, and referrals to local treatment centers.
For emotional or mental-health crises
988 Suicide & Crisis Lifeline – dial 988
You can call, text, or chat online. They handle not only suicidal thoughts but also overwhelming stress, panic, or substance-related crises.
For peer-to-peer recovery support
Alcoholics Anonymous (AA) – Find local or online meetings at aa.org
SMART Recovery – A science-based, non-12-step alternative at smartrecovery.org
Quick Safety Notes
If you’ve been drinking heavily, don’t quit suddenly without talking to a doctor. Withdrawal can be medically dangerous.
If you’re on prescription medication for addiction recovery, never adjust or stop it on your own—always coordinate with your healthcare team.
If you ever feel you might harm yourself or someone else, call 911 or 988 right away.
Unlearning the Loop
A Guided Practice for Understanding and Rewiring Addiction
Purpose:
This worksheet helps you understand why cravings feel powerful and how to interrupt them safely. It pairs with the article Addiction: The Loop Between Pain and Relief and is best used alongside your doctor or therapist, especially if alcohol or multiple substances are involved.
1. Understand Your Loop
Trigger → Behavior → Relief
Trigger (what starts it?)Behavior (what you do)Relief/Reward (what you feel)Example: stress after workPour a drinkCalm, escape, comfortExample: boredom at nightScroll, snack, smokeDistraction, stimulation
Reflection:
What does your brain believe this habit does for you?
Write a short phrase:
“My brain learned that when I feel ________, doing ________ gives me ________.”
2. Recognize the Lure
When a craving shows up, the brain sends a false message:
“You need this to feel safe.”
Answer these questions honestly:
Where in your body do you feel the craving? (throat, chest, stomach?)
How long does it usually last before fading?
What emotion usually hides underneath—stress, loneliness, exhaustion, anxiety?
3. Bring in Curiosity (Dr. Jud Brewer’s Mindful Pause)
The next time you notice an urge:
Pause. Don’t react—observe.
Notice. What does it feel like? Heat, tightness, restlessness, salivation?
Name it. “This is craving.” (Naming moves it from instinct to awareness.)
Get curious. What happens if I breathe and just watch this feeling for 90 seconds?
Rate the urge after two minutes:
0 = gone, 10 = unbearable.
Write your number here: _____
Repeat daily for one week and notice if the number changes.
4. Rewire the Pathway
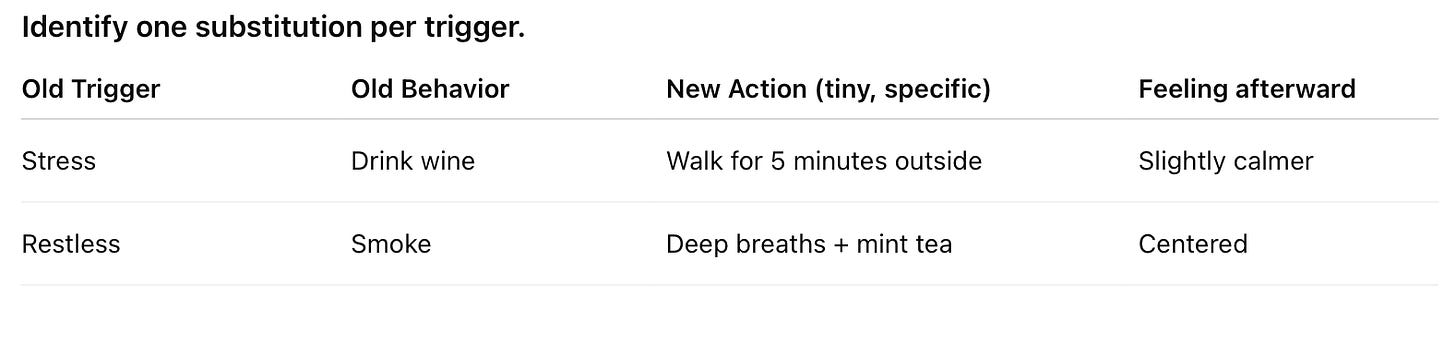
Identify one substitution per trigger.
The goal isn’t perfection—it’s repetition. Every time you choose the new action, your brain lays a new track.
5. Work With Your Doctor (Especially for Alcohol)
Medical safety first. If you drink daily or heavily, never stop cold turkey without supervision. Alcohol withdrawal can be dangerous.
Ask your physician about:
Naltrexone (reduces the reward of drinking)
Acamprosate (steadies mood and sleep after quitting)
Gabapentin or topiramate (for withdrawal or persistent cravings)
Bring this worksheet to your next visit. It helps your doctor understand your patterns and match treatment safely.
6. Build the New Reward System
Craving teaches your brain that comfort comes from a substance. You can teach it something better.
List three non-harmful sources of relief:
Each time you reach for one instead of the old habit, you’re teaching your brain: relief lives here instead.
7. Reflection Journal
What surprised you about your cravings this week?
When did you feel most in control?
What’s one situation you’d like to handle differently next time?
Who could you reach out to for support before the next wave hits?
Key Reminders
Craving ≠ emergency. It’s a passing body signal.
Awareness breaks the loop faster than resistance.
Healing is safer and more successful when guided by medical and social support.
References:
Volkow ND, Boyle M. Neuroscience of Addiction: Relevance to Prevention and Treatment. Am J Psychiatry. 2018;175(8):729-740. doi:10.1176/appi.ajp.2018.17101174
Volkow ND, Michaelides M, Baler R. The Neuroscience of Drug Reward and Addiction. Physiol Rev. 2019;99(4):2115-2140. doi:10.1152/physrev.00014.2018
Brewer JA, Mallik S, Babuscio TA, et al. Mindfulness training for smoking cessation: results from a randomized controlled trial. Drug Alcohol Depend. 2011;119(1-2):72-80. doi:10.1016/j.drugalcdep.2011.05.027
Brewer JA, Elwafi HM, Davis JH. Craving to quit: psychological models and neurobiological mechanisms of mindfulness training as treatment for addictions. Psychol Addict Behav. 2013;27(2):366-379. doi:10.1037/a0028490
Prochaska JJ, Benowitz NL. Current advances in research in treatment and recovery: Nicotine addiction. Sci Adv. 2019;5(10):eaay9763. Published 2019 Oct 16. doi:10.1126/sciadv.aay9763
Potenza MN, Sofuoglu M, Carroll KM, Rounsaville BJ. Neuroscience of behavioral and pharmacological treatments for addictions. Neuron. 2011;69(4):695-712. doi:10.1016/j.neuron.2011.02.009
Lomas C. Neurobiology, psychotherapeutic interventions, and emerging therapies in addiction: a systematic review. J Addict Dis. Published online December 17, 2024. doi:10.1080/10550887.2024.2440184
Reichert, R. A., Boos, F. Z., Legal, E. J., de Mello, C. B., De Micheli, D., & Lopes, F. M. (2025). Neuropsychological interventions for the treatment of substance use disorders. In R. A. Reichert, A. L. M. Andrade, & D. De Micheli (Eds.), Neuropsychology and substance use disorders: Assessment and treatment (pp. 579–591). Springer Nature Switzerland AG.
Volkow ND, Blanco C. Substance use disorders: a comprehensive update of classification, epidemiology, neurobiology, clinical aspects, treatment and prevention. World Psychiatry. 2023;22(2):203-229. doi:10.1002/wps.21073




I'm nearly 4 years sober after drinking for 50 years. I also attend AA meetings and, more importantly in my mind, attend and facilitate Smart Recovery meetings a few days a week.
While I truly appreciate the way you presented the underlying mechanism of addiction, I view the use of medication a useful crutch in many circumstances, but definitely secondary to effective personal and group therapies.
I got sober without meds, and I know people who, sadly, did not take full advantage of the use of pills or could not find meds that helped turn down that volume adequately for them.
Again, this discussion is, in my opinion, critically necessary for society and individuals to consider. But the foremost task for us humans is to realize the way addiction lies to us, and the promise and potential of introspection and internal growth to handle life as we know it.
I hope this didn't come out either too jumbled or poorly typed. I felt compelled to respond first thing in reading today's note and am entering this in my damn phone!
Most of us, unfortunately, feel compelled to self-medicate in some form or another (besides caffeine), albeit it’s more or less ‘under control’. And there are various forms of self-medicating, from the relatively mild to the dangerously extreme, that include non-intoxicant-consumption addictions, like chronic shopping/buying, gambling, pornography or over-eating — especially sugar and salt snack consumption.
If such self-medicating forms are anything like drug intoxication or substance addiction, it should follow that: the greater the induced euphoria or escape one attains from it, the more one wants to repeat the experience; and the more intolerable one finds their non-self-medicating reality, the more pleasurable that escape will likely be perceived. In other words: the greater one’s mental pain or trauma while not self-medicating, the greater the need for escape from one’s reality — all the more addictive the euphoric escape-form will likely be.
With food, the vast majority of obese people who considerably over-eat likely do so to mask mental pain or even PTSD symptoms. I utilized that method myself during much of my pre-teen years, and even later in life after ceasing my (ab)use of cannabis or alcohol. I don’t take it lightly, but it’s possible that someday I could instead return to over-eating.
In the book (WHAT HAPPENED TO YOU? Conversations on Trauma, Resilience and Healing) he co-authored with Oprah Winfrey, Dr. Bruce D. Perry (M.D., Ph.D.) writes in regards to self-medicating trauma, substance abuse and addiction:
“For people who are pretty well-regulated, whose basic needs have been met, who have other healthy forms of reward, taking a drug will have some impact, but the pull to come back and use again and again is not as powerful. It may be a pleasurable feeling, but you’re not necessarily going to become addicted. Addiction is complex. But I believe that many people who struggle with drug and alcohol abuse are actually trying to self-medicate due to their developmental histories of adversity and trauma.”